You don’t have to live with painful periods. You also don’t have to fear getting your period. AND, wait for it, you don’t need to take birth control.
I used to live in fear of my period. Sooo much fear. I did not know when it would come, how painful it would be, if I would pass out or even have diarrhea. One thing I did know is that the day I got my period would be an entire day of me out for the count, next to a toilet, praying to God that I would just pass out from the pain. I was diagnosed with PCOS at the age of 18. I probably went undiagnosed for years like many women out there.
So ladies, I understand. PCOS can be a b****.
How can I know if I have PCOS?
PCOS or Polycystic Ovary Syndrome is a common hormone (or endocrine) disorder in women. It affects 5-20% of women globally. That does not include other hormonal imbalance issues. That statistic is mind-blowing to me.
To better understand hormone disorders like PCOS, it’s helpful to fully understand what a hormone is.
A hormone is a chemical messenger that carries messages through your bloodstream to your organs, skin, muscles and tissues. They literally receive a message and then carry that message.
So, hormones produce or perform an action because something in the body told them to do so. They are a secondary issue” 🤯
The big kicker about PCOS is that up to 70% of PCOS cases are UNDIAGNOSED!
Why is that? Well, PCOS can be hard to diagnose.
Medically, women are diagnosed with PCOS if they meet two of the three following features:
- Hyperandrogenisms- clinical signs are hirsutism (or body or facial hair growth), and/or biochemical signs are high levels of androgens, such as cortisol, testosterone or DHEA-S
- Ovulatory dysfunction-irregular periods or not ovulating correctly (missing periods or not ovulating at all!)
- Visible cysts in the ovaries on an ultrasound.
However, symptoms of PCOS can also include:
- Irregular periods, missed periods or very light periods
- Abnormal hair growth (think face, stomach, back, chest)
- Acne or oily skin
- Obesity or weight gain, especially around the belly
- Darkening of the skin
- Cysts
- Skin tags
- Thinning hair or male pattern baldness
- Infertility
So why are 70% undiagnosed?
Well, when I am talking with women, I realize many women may be undiagnosed because they do not have complete testing, hormonally speaking.
How do I confirm if I have PCOS?
There are several ways of testing hormones: blood, saliva, and urine. Testing hormones by blood are the most common way to test hormones, but they only offer a snapshot of your hormone levels at a single moment—they don’t always reveal the full picture.
If you have had blood testing, look at your lab results. What did they test? Did they test your testosterone levels? Did they test your cortisol, DHEA, insulin, estrogens, or progesterone? Did they test Androstenedione (A4)?
If not, you are not getting the full picture. Are you possibly one of the undiagnosed due to incomplete testing?
For hormone imbalances in women, I like to test hormones by blood and also by urine using a DUTCH test (Dried Urine Test for Comprehensive Hormones.)
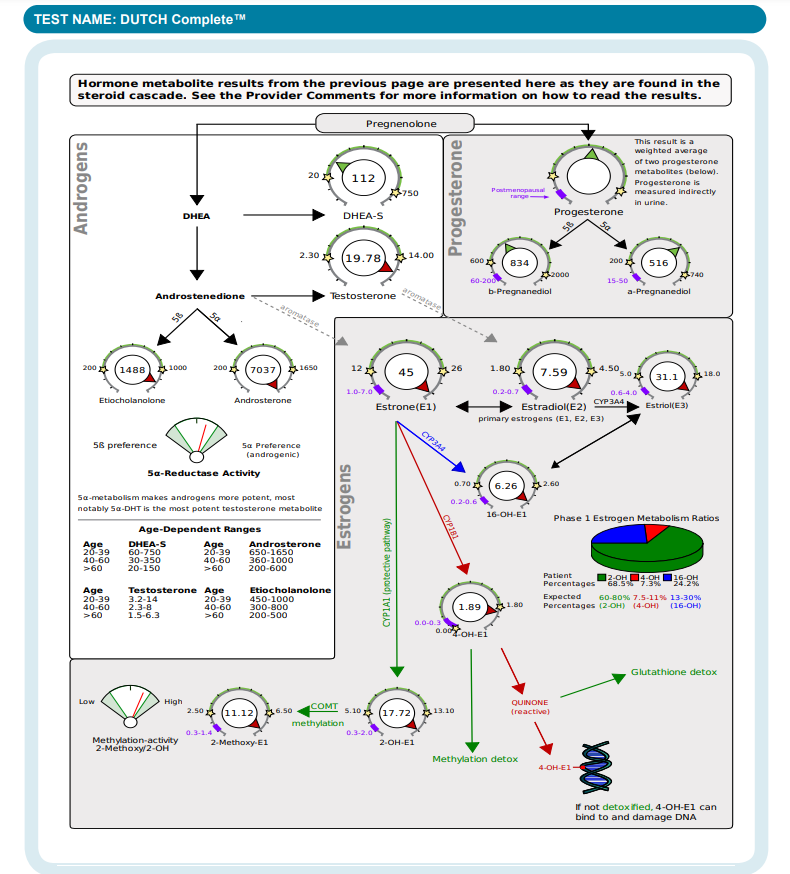
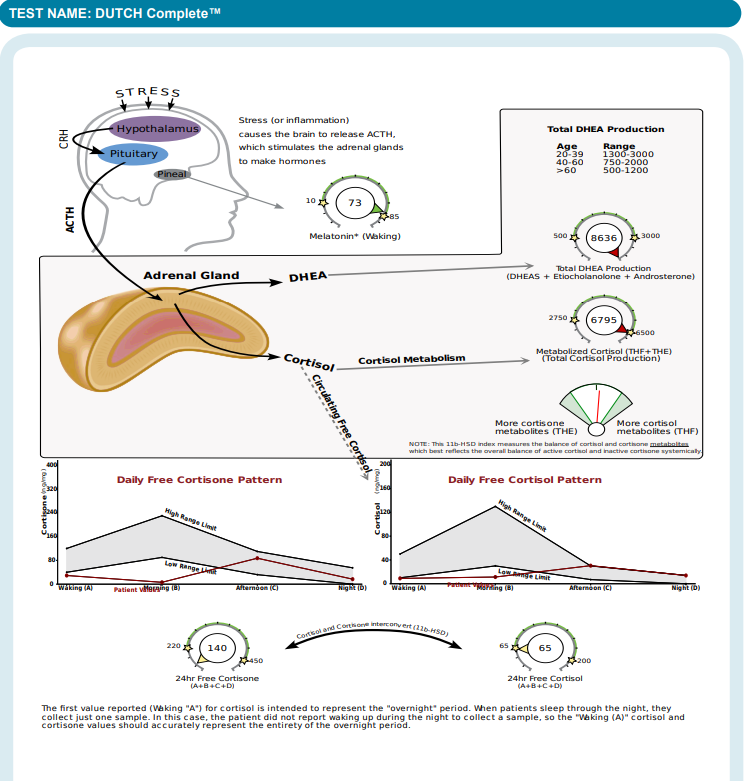
This is done over a 24-hour period so we can check your primary hormones, but also your hormone metabolites and cortisol pattern.
We have hormone metabolites, or the metabolism and breakdown of your primary hormones. Hormone metabolites and pathways are important. They each have their purpose in the body. You need a better picture of what is going on inside your body.
You can see these in the pictures below of a DUTCH test sample. Each “gear” represents a primary hormone or a hormone metabolite and their pathways. For example, A4 is the most abundant blood steroid metabolite in patients with PCOS. Could A4 be high, but testosterone levels be normal? Yes! If your doctor only tested your testosterone level and your testosterone came back as “normal”, your high A4 level may have been missed. A4 level is important for women struggling with PCOS because it tells us how that testosterone is metabolizing in your body.
See how much more comprehensive this test is?!
“Why doesn’t my medical doctor run this test?” Well, 1) they may not know what to do with the results (I hear this quite often) and/or 2) the test is not covered by insurance.
What causes PCOS, and is it something that can be prevented?
Did you know that PCOS develops over time, not overnight? Research shows that “PCOS is closely associated with persistent low-grade inflammation.” Think about what the word ‘persistent’ means.**
PCOS did not just happen in one day, it happened after a period of time of inflammation in the body. If you have not attended one of my inflammation talks before– please check out my events page.
We need to figure out what is triggering inflammation in your body! With my patients with PCOS and really any other hormonal imbalance, it is usually multiple root causes or inflammatory triggers.
Inflammation triggers in the body often come from what we call the ‘3T’s’—thoughts (stress), traumas (subluxations in the spine causing nervous system dysfunction), toxins (gut issues, environmental toxins, makeups, foods, etc).
Your body is like a Swiss watch where every gear (or organ system) affects another.
Could it be your diet, could it be stress, could it be mold, could it be your gut? Every single woman is different. We all have different stressors and inflammatory triggers. You won’t know yours until you test.
With The Wellness Way we have a motto, “We don’t guess, we test!”
For example, research shows that women with PCOS often have an imbalanced gut microbiome (the trillions of bacteria living in the digestive system) and less bacterial diversity. This imbalance can affect hormone levels, inflammation, and even insulin resistance, all of which are key players in PCOS.
Your gut bacteria can influence how your body processes hormones and communicates with the brain. In fact, an unhealthy gut might contribute to the hormonal chaos seen in PCOS by affecting bile acids, metabolism, and inflammation. So, taking care of your gut health may be an important part of managing PCOS!
How does PCOS affect your life?
PCOS doesn’t just impact your ovaries—it affects your whole body, both now and in the long run. Women with PCOS often experience a mix of issues:
- Reproductive Health: PCOS can cause infertility, pregnancy complications, and irregular cycles, making family planning more challenging.
- Metabolic Challenges: Women with PCOS are at a higher risk for type 2 diabetes and heart disease due to insulin resistance. Excess insulin can kick-start the ovaries into making more androgens (male hormones), leading to a cycle where hormone imbalances and metabolic issues keep feeding off each other, making symptoms worse over time
- Mental Health Struggles: Women with PCOS often struggles with anxiety or depression due to the hormonal imbalances that affect mood regulation. These emotional challenges can be compounded by the physical symptoms of PCOS, such as weight gain and acne, leading to lower self-esteem and increased stress.
So, when I sit down at talk to women in consultations, whether that be in person or online, we talk about it ALL! I am discussing with them possible inflammatory triggers– diet, lifestyle, stress, gut issues, etc. Understanding your unique triggers is how we can help you break the cycle and take back control of your health again.
What are the best treatment options for managing PCOS symptoms naturally?
Find your WHY. Why are your hormones imbalanced? What is triggering them?
Once you figure out your why, THEN you will know HOW to address them in a way unique to you.
1. Do you need dietary changes? Processed carbs, sugary snacks, and inflammation-triggering foods could be making your symptoms worse. There is no one diet fits all for women with PCOS. Your diet needs to be approach uniquely to you and your needs. Are you eating enough healthy fats? Foods rich in omega-3 fatty acids can “help reduce the production of pro-inflammatory mediators, such as cytokines…reducing inflammation.”
2. Do you need to make lifestyle changes? Toxins in our environment may play a bigger role in PCOS than you think! Think about all the products you use every day– from your face lotion to your shampoo, to the utensils you use to cook. It all adds up. These toxins can affect your body’s delicate hormonal balance, potentially leading to PCOS. Let’s be real, we live in a pretty toxic world. Limit your toxin exposure where and when you can.
3. Do you need more testing? Have your hormones been tested properly? Has your insulin been tested? Have your hormones been tested properly? Has your insulin been tested? Do you have other inflammatory triggers, such as food allergies or gut issues that need to be addressed? Do you have mold exposure affecting inflammation in your body? You won’t know until you test.
4. Stay Committed to Long-Term Changes: Making changes to your diet and lifestyle are not easy and it is not a quick fix. I like to tell my patients that it takes a minimum of 3 months for them to feel and see changes. The first month your body doesn’t know what is happening, the second month it’s like “alright, I get it” and by the third month it’s starting to know the new normal. Because your menstrual cycle is exactly that– a cycle. Every week is different, so ALL of your hormones and tissues need to adapt to changes
PCOS management takes effort and time, and women do not have a guide to help them– it is all too common for women to be put on birth control. Birth control is a band-aid. It is not addressing your root causes. As women, we are not taught how we have multiple hormones and how diet and our lifestyle play a role in our hormonal health and what to do about it.
And I get it, I was put on birth control for 10 years because it was my doctor’s answers for helping regulate my periods and helping with the pain. I didn’t know what else to do. And birth control came with a whole different list of side effects. Side note: If you have not read the book, “This is Your Brain on Birth Control,” read it!
I want you to know that I am here to help guide you and help find you answers. You don’t have to do it alone. It just starts with a conversation, let’s talk! Book a discovery call!
